Contents
Have you ever wondered how medical devices can so precisely monitor your heartbeat or blood oxygen levels? Welcome to the world of biomedical instrumentation—where engineering meets healthcare to improve lives. In this article on the Tech4Ultra Electrical website, you’ll learn how biomedical devices, biosensors, and transducers work together inside medical instruments to deliver accurate diagnostics and safe treatments. If you’re curious about the technology saving lives every day, you’re in the right place.
What Is Biomedical Instrumentation?
Biomedical instrumentation refers to the design, development, and use of devices and systems that help monitor, diagnose, and treat medical conditions. These instruments convert physiological data—like heart rate, brain activity, or oxygen levels—into signals that doctors and medical staff can read and analyze. At its core, it’s where engineering and medicine intersect to improve patient care.
Its importance in healthcare can’t be overstated. With the rise of modern medicine, biomedical devices have become essential in everything from routine checkups to critical surgeries. Think of machines like ECG monitors, blood glucose meters, or MRI scanners—all of them are products of biomedical instrumentation. These medical instruments provide real-time, accurate information, which allows doctors to make better, faster decisions, often saving lives in the process.
The journey of biomedical instrumentation began in the early 20th century. Back then, most tools were mechanical or analog. Over time, thanks to advancements in electronics and computing, biosensors and transducers were introduced—allowing for more precise and automated measurements. Today, we’re seeing even more sophisticated systems integrated with AI, wireless communication, and miniaturization, making devices smarter, smaller, and more accessible than ever.
So next time you see a patient hooked up to a monitor, remember: there’s a whole field of science behind that blinking screen—biomedical instrumentation.
Read Also: Arduino vs Raspberry Pi: Which One Should You Use?
Key Functions of Biomedical Instruments
At first glance, biomedical instruments may just look like high-tech boxes with blinking lights—but every one of them plays a crucial role in patient care. These devices are more than tools; they’re lifesavers, thanks to four main functions: measurement, monitoring, diagnosis, and therapy assistance.
Measurement is the foundation of all biomedical instrumentation. These systems gather physiological data such as heart rate, blood pressure, or oxygen saturation using biosensors. The information is then converted by transducers into electrical signals that can be processed and analyzed.
Monitoring comes next. This is the continuous observation of a patient’s vital signs over time. Think of a heart monitor in an ICU—it doesn’t just measure once; it tracks changes in real-time to alert medical staff of any danger.
Diagnosis is where things get even more interesting. By interpreting the data gathered from biomedical devices, doctors can pinpoint health issues more accurately. An ECG, for example, can detect abnormal heart rhythms that may indicate serious conditions.
Finally, there’s therapy assistance. Some medical instruments don’t just diagnose; they actively help treat patients. Devices like insulin pumps, ventilators, and pacemakers are excellent examples—they respond to a patient’s condition and adjust their output accordingly to aid recovery.
These four pillars make biomedical instruments indispensable in today’s healthcare system.
Types of Biomedical Signals and Parameters
Understanding how the body communicates is essential in healthcare—and that’s exactly what biomedical instrumentation helps us decode. These devices work by picking up different types of signals that reflect what’s happening inside the body. Whether it’s the beat of your heart, the air in your lungs, or the sugar in your blood, each signal tells a story. Let’s break them down into three key categories: electrical, non-electrical, and chemical.
Electrical signals are probably the most recognized. Devices like the ECG (electrocardiogram), EMG (electromyogram), and EEG (electroencephalogram) measure the electrical activity of the heart, muscles, and brain, respectively. These biomedical devices rely on biosensors and transducers to detect small voltage changes and convert them into readable data. It’s amazing how something as subtle as a brainwave can be turned into useful information using the right medical instruments.
Non-electrical signals include parameters like body temperature, blood pressure, and respiration rate. Measuring these might seem simple, but accuracy is everything. A one-degree change in body temperature can signal infection. A dip in blood pressure might warn of internal bleeding. These signals are captured using pressure sensors, thermistors, and airflow monitors—each carefully designed with biomedical instrumentation principles.
Then, we have the chemical signals, which are just as critical. Monitoring blood glucose levels in diabetics or pH balance in intensive care patients can mean the difference between life and death. These measurements are taken using advanced biosensors that react chemically with the sample and output a signal through a transducer.
Each signal, no matter how small or subtle, contributes to a much bigger picture. And thanks to modern biomedical instrumentation, we now have the tools to capture, understand, and act on these signals faster than ever before. It’s like having a translator for your body, working 24/7.
Core Components of a Biomedical Instrumentation System
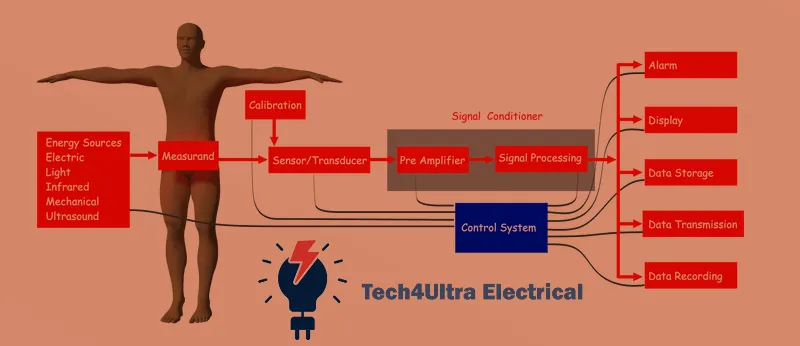
Every effective biomedical instrumentation system has one job: translate what the body is saying into something we can understand. It may sound simple, but the process involves several tightly integrated components—each playing a critical role in turning raw biological signals into meaningful information. Let’s walk through the core elements step-by-step.
Transducers and Biosensors
It all begins with transducers and biosensors. A transducer is a device that converts one form of energy into another—typically, physical or chemical signals into electrical signals. A biosensor takes it a step further, combining a biological element (like an enzyme or antibody) with a sensor to detect specific substances such as glucose or pH levels. These components are the ‘ears’ of biomedical devices, picking up tiny signals from the body and making them measurable.
Signal Conditioning (Amplification and Filtering)
Once a signal is captured, it’s often too weak or noisy to be useful. This is where signal conditioning steps in. Amplification boosts the signal strength, while filtering removes unwanted noise. Without this stage, an ECG reading would look like static on a TV screen—chaotic and unreadable. Signal conditioning ensures the clarity and accuracy of the data before it moves forward in the system.
Analog-to-Digital Conversion
Most medical instruments work with digital systems, but the human body operates in analog. That’s why analog-to-digital converters (ADCs) are essential. They transform continuous biological signals into digital data that computers and microcontrollers can process. It’s a silent but vital bridge between biology and technology.
Data Processing and Display
After digitization, the signal is processed—either in real-time or after collection. Data processing can involve anything from basic statistical analysis to advanced pattern recognition. Then comes the display, which presents the results to healthcare professionals via monitors, graphs, or even mobile apps. A well-designed display can be the difference between a life saved and a detail missed.
Use of AI and Real-Time Data Interpretation
Modern biomedical devices increasingly leverage artificial intelligence to interpret data in real time. For instance, smart algorithms can analyze an ECG and instantly alert staff if they detect signs of a heart attack. This combination of real-time monitoring and AI-powered insights is pushing biomedical instrumentation to the next level—making diagnostics faster, smarter, and more accurate than ever before.
Together, these components form the backbone of modern biomedical instrumentation systems, turning complex biological data into life-saving decisions.
Common Biomedical Devices and Their Applications
The beauty of biomedical instrumentation is how it blends into every corner of modern healthcare—often without us even noticing. From routine checkups to emergency interventions, biomedical devices play crucial roles in diagnosis, treatment, and long-term monitoring. Let’s look at the most common devices and how they improve lives every day.
Diagnostic Devices
When it comes to identifying health issues, diagnostic tools are the first line of defense. These medical instruments gather crucial data, helping doctors make accurate decisions.
- ECG (Electrocardiogram): Measures the electrical activity of the heart. It can detect arrhythmias, heart attacks, and more in just minutes.
- EMG (Electromyogram): Records the electrical signals of muscles. It helps diagnose nerve dysfunctions and muscular disorders.
- EEG (Electroencephalogram): Tracks brainwave activity. Doctors use it to identify epilepsy, sleep disorders, and brain injuries.
- Imaging Devices: X-rays, CT scans, and MRI machines use different technologies to visualize internal organs. MRI, for instance, provides detailed 3D images without harmful radiation, making it a favorite for soft tissue evaluation.
All of these devices depend on high-performance transducers and biosensors to pick up accurate signals, which are then processed through advanced biomedical instrumentation systems.
Therapeutic Devices
Once a diagnosis is made, treatment often involves therapeutic biomedical devices. These devices don’t just support health—they actively save lives.
- Pacemakers: Implanted into the chest to regulate abnormal heart rhythms. They monitor heart signals and deliver electrical impulses when needed.
- Infusion Pumps: Deliver fluids like medication, insulin, or nutrients directly into a patient’s bloodstream at controlled rates. They’re vital in ICUs and for patients with chronic conditions.
What makes these devices stand out is their precision. Using real-time data and feedback systems, they can adapt to a patient’s condition dynamically, which is the core promise of modern biomedical instrumentation.
Monitoring Devices
Ongoing care often relies on continuous monitoring. These tools track patient vitals to ensure that everything stays within safe limits.
- ICU Monitors: Constantly display heart rate, oxygen saturation, blood pressure, and more. Alerts are triggered the moment anything abnormal is detected.
- Wearable Health Trackers: From smartwatches to fitness bands, these devices are the new frontier. They measure heart rate, sleep cycles, activity levels, and even blood oxygen—bringing biomedical devices right to your wrist.
Wearables often include biosensors and smart transducers, powered by cloud data and AI for personalized health insights. What used to require a hospital stay can now be tracked 24/7 with a tiny device at home.
Each of these categories—diagnostic, therapeutic, and monitoring—represents a different aspect of how biomedical instrumentation supports health. Together, they form a powerful ecosystem that’s making healthcare more efficient, accessible, and proactive.
Biomedical Transducers and Biosensors
If you’ve ever used a digital thermometer or worn a heart rate monitor, you’ve already experienced the power of biomedical transducers and biosensors. These tiny components are the heart of many biomedical devices, quietly converting body signals into readable data for doctors—or even for you.
Working Principles
The concept is simple but brilliant. A transducer detects a physical or chemical signal—like pressure, temperature, or a chemical concentration—and transforms it into an electrical signal. A biosensor works similarly but adds a biological layer, such as an enzyme or antibody, to interact with specific substances like glucose or pH levels. The combined response gets translated through the transducer for further processing.
Types of Transducers and Biosensors
- Piezoelectric: These use mechanical stress to produce an electric charge. They’re often used in ultrasound imaging or blood pressure monitors.
- Optical: Light is the key here. Changes in light absorption or reflection can indicate oxygen levels or detect pathogens in a sample.
- Chemical: These are common in glucose monitors. They use reactions between biological molecules and analytes to produce a measurable signal.
Each type serves a unique role in biomedical instrumentation, depending on what needs to be measured and how sensitive or specific the data must be.
Wearable and Implantable Sensors
Today’s trend is all about mobility and real-time feedback. Wearable biosensors—like fitness trackers or continuous glucose monitors—offer round-the-clock health data without hospital visits. Meanwhile, implantable transducers are used in devices like pacemakers and neurostimulators, providing long-term monitoring from inside the body.
Both types rely on innovations in material science, power efficiency, and wireless communication—making biomedical instrumentation not only smarter but more human-friendly than ever before.
Safety, Standards, and Regulatory Considerations
When it comes to biomedical instrumentation, precision isn’t the only priority—safety is equally vital. Any device that comes into contact with the human body must meet strict regulations to ensure it doesn’t harm the very people it’s meant to help.
Patient Safety and Electrical Isolation
Electrical isolation is one of the most important safety principles in biomedical devices. Since these tools often interface directly with the human body, even minor electrical faults can be dangerous. Devices must be designed to prevent leakage currents and isolate sensitive electronics from patient contact areas. This is especially critical in devices like ECGs or pacemakers where direct electrical interaction is part of their function.
International Standards (ISO, IEC, FDA)
To ensure global safety and compatibility, medical instruments must comply with standards from organizations like ISO (International Organization for Standardization), IEC (International Electrotechnical Commission), and the FDA (U.S. Food and Drug Administration). For example, ISO 13485 outlines quality management for medical devices, while IEC 60601 covers the safety and performance of electrical equipment in healthcare settings. These standards aren’t optional—they’re legal requirements in most countries.
Data Privacy and Cybersecurity in Medical Devices
Modern biomedical devices often store or transmit sensitive patient data, making cybersecurity a top concern. Whether it’s a wearable heart monitor or an implantable sensor, protecting health information from unauthorized access is non-negotiable. That’s why data encryption, user authentication, and secure communication protocols are essential components of today’s biomedical instrumentation systems.
From hardware design to software integrity, every step in the development of biomedical devices is governed by safety and ethics—because when it comes to health, there’s no room for error.
Challenges in Biomedical Instrumentation Design
Designing biomedical devices isn’t as simple as fitting electronics into a sleek casing. Behind every successful tool lies a long list of engineering challenges—each with its own set of compromises. Let’s explore a few that stand out the most.
Accuracy vs. Invasiveness
One of the biggest dilemmas in biomedical instrumentation is balancing accuracy with patient comfort. The more invasive a device, the more precise data it often delivers. But invasiveness comes with risks—infection, discomfort, and limited usage time. Non-invasive alternatives like wearable biosensors are safer but may not offer the same data fidelity. Designers must constantly weigh clinical value against the practical realities of use.
Noise and Signal Interference
In the real world, signals don’t come clean. Electrical noise, motion artifacts, and interference from other medical instruments can distort data, especially in sensitive applications like EEG or EMG. Signal conditioning circuits—amplifiers, filters, and shielding—are essential to minimize errors. Still, even the best systems can struggle in noisy environments like hospitals or operating rooms.
Power Consumption and Portability
As biomedical devices become smaller and more portable, managing power becomes critical. Wearables and implantables, in particular, must run on minimal energy while maintaining functionality. That means using low-power electronics, efficient data transmission protocols, and smart power-saving modes—all without compromising performance.
Solving these challenges is what pushes innovation forward. In fact, many breakthroughs in biomedical instrumentation come from tackling these exact problems—making devices not just smarter, but safer and more usable, too.
Watch Also: Understanding the Schottky Effect: Field Enhanced Thermionic Emission Explained in Depth
Emerging Trends and Future Directions
As technology continues to evolve, so does the potential of biomedical instrumentation. The tools we once used just to monitor are now starting to predict, adapt, and even communicate in ways we never imagined. Here’s a glimpse at the cutting-edge trends that are transforming how biomedical devices are designed and used.
Telemedicine and Remote Monitoring
The shift toward telemedicine has fueled rapid innovation in remote medical instruments. Patients can now be monitored at home with wearable biosensors that send real-time data to doctors. From tracking heart rhythms to managing chronic diseases, remote monitoring allows for faster interventions and fewer hospital visits—perfect for aging populations and underserved areas.
AI Integration and Predictive Analytics
Artificial intelligence is becoming a game-changer in biomedical instrumentation. AI can detect subtle patterns in biosignals that human eyes might miss. For example, smart algorithms can analyze ECG data to predict arrhythmias before symptoms appear. With predictive analytics, biomedical devices are shifting from reactive to proactive tools in healthcare.
IoT and Connected Healthcare
The Internet of Things (IoT) is weaving together an entire ecosystem of connected biomedical devices. From smart insulin pens to cloud-linked ICU monitors, devices can now communicate with each other and with electronic health records. This connectivity improves coordination among healthcare providers, reduces errors, and supports real-time decision-making.
Personalized Biomedical Devices
We’re entering the age of personalized medicine—and that means customized biomedical instrumentation. Devices are being tailored to individual needs, from 3D-printed prosthetics to adjustable pacemakers. This trend not only enhances comfort but also improves clinical outcomes, especially in long-term care and rehabilitation.
These emerging trends point to a future where biomedical devices are smarter, more connected, and increasingly focused on individual care. It’s an exciting time for innovation—and even more so for patients whose lives are being transformed by these technologies every day.
Conclusion
Biomedical instrumentation has completely reshaped modern medicine. From simple sensors to complex diagnostic machines, these tools have become the silent backbone of healthcare. Throughout this guide, we explored how biomedical devices measure vital signs, assist in therapy, and provide real-time monitoring through biosensors and transducers.
We looked into how medical instruments are designed to balance accuracy, safety, and usability. We also covered the critical role of international standards, data security, and the challenges that engineers face—from minimizing power consumption to managing signal noise.
Most exciting of all are the future trends. As AI, IoT, and personalized healthcare continue to evolve, so too will the power and scope of biomedical instrumentation. Devices are getting smaller, smarter, and more connected—bringing care to where the patient is, not just where the hospital is.
In short, the fusion of biology and technology isn’t just saving lives—it’s redefining how we understand and deliver healthcare.
FAQs
What is the introduction of biomedical instrumentation?
Biomedical instrumentation refers to the field that designs and develops tools to monitor and analyze physiological functions in the human body. It combines engineering, biology, and medicine to create biomedical devices like ECGs, MRI scanners, and wearable sensors that help in diagnosis, therapy, and monitoring.
What is the introduction of instrumentation?
Instrumentation is the science of measuring and controlling physical quantities. In healthcare, it’s a vital component of biomedical instrumentation, enabling accurate detection and analysis of signals such as temperature, pressure, and electrical activity using sensors and transducers.
What is the introduction of biomedical equipment?
Biomedical equipment includes the medical instruments and machines used in hospitals and clinics to diagnose, monitor, and treat patients. These range from imaging systems like CT scanners to life-support machines like ventilators and infusion pumps.
What is biomedical instrumentation short notes?
Biomedical instrumentation involves the use of biosensors, transducers, and electronic systems to convert physiological signals into readable outputs. It supports areas such as diagnostics, patient monitoring, and therapeutic control, making it a critical part of modern healthcare systems.

1 thought on “SCR turn-on time Explained: Complete Guide to Switching and Turn‑Off Characteristics”